Achilles Rupture
What is the Achilles Tendon?
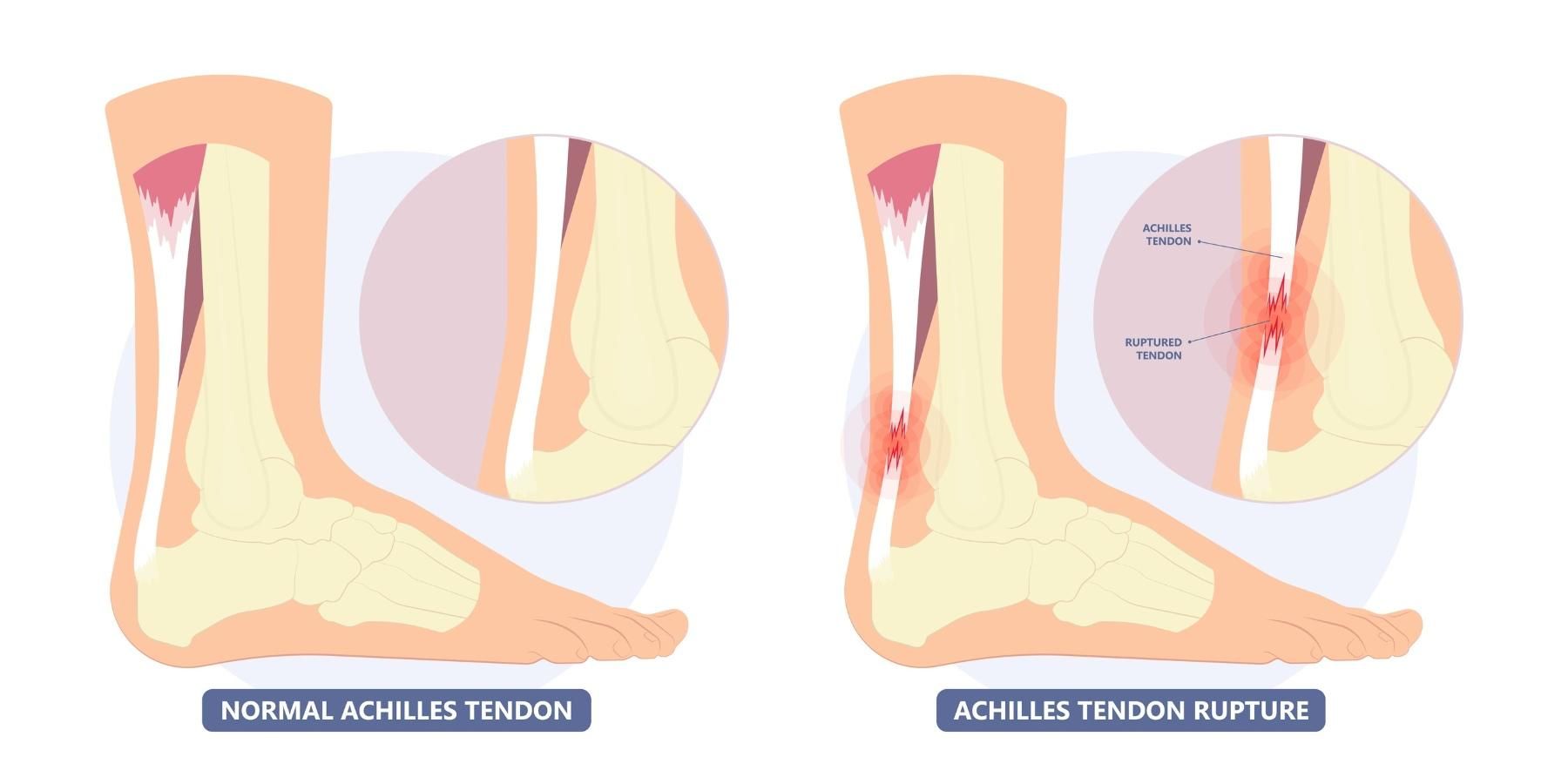
The Achilles tendon is the large tendon at the back of the heel. It is an important tendon for walking. It can tear (or rupture) with forceful push, such as in sports like sprinting, tennis, basketball or football.
What is Achilles Rupture?
Achilles rupture refers to a tear or break in the Achilles tendon. When this tendon tears, it can cause sudden pain, loss of function, and difficulty moving. Achilles rupture can occur partially or completely, depending on the severity of the injury.

Impact of Achilles Rupture on Anatomy and Health
When the Achilles tendon ruptures, it disrupts the lower leg biomechanics. This leads to several anatomical and functional changes, including:
- Loss of Mobility: The Achilles tendon is essential for pushing off the ground when walking or running. A rupture can significantly impair your ability to perform these basic movements.
- Pain and Swelling: The area around the rupture typically becomes painful, swollen, and tender to the touch.
- Weakness in the Leg: Without a fully functioning Achilles tendon, the calf muscles lose their ability to generate force, leading to leg weakness.
- Gait Alteration: The injury forces you to adopt compensatory walking or standing patterns, which can strain other parts of the leg or body over time.
Risk Factors for an Achilles Rupture
Achilles ruptures often occur in men in their 20s to 50s who play high-energy sports in their spare time.
- Medication: Some medications, such as steroids or steroid injections, can cause weakness of the tendon
- Trauma: Occasionally, the Achilles tendon is ruptured by a direct laceration
Causes of an Achilles Rupture
Achilles tendon rupture occurs when the tendon experiences excessive stress or strain that exceeds its capacity to withstand the force. Common causes include:
- Sudden Movements or Trauma: Rapid, explosive movements, such as jumping, sprinting, or pivoting, can place immense pressure on the tendon and cause a tear.
- Overuse or Repeated Stress: Repeated high-intensity activities without adequate rest can weaken the tendon, increasing the likelihood of rupture.
- Improper Technique or Footwear: Poor athletic techniques or unsupportive shoes during exercise can strain the tendon unnecessarily.
- Age-Related Degeneration: As people age, the Achilles tendon becomes less flexible and less able to handle stress, making it more prone to rupture.
- Direct Injury: A sharp blow to the back of the ankle can cause the tendon to tear.
- Medication Side Effects: Fluoroquinolone antibiotics or corticosteroid injections can weaken tendons, increasing the risk of rupture.
- Underlying Health Conditions: Diabetes, rheumatoid arthritis, or other chronic conditions can compromise the structural integrity of the tendon.
Symptoms of an Achilles Rupture
Achilles ruptures typically present with:
- A feeling someone has kicked you in the back of the heel
- Difficulty walking and unable to stand flatfooted
- Pain, swelling and/or bruising over the back of the heel
Prevention of Achilles Rupture
Preventing an Achilles tendon rupture involves maintaining strong, flexible, and healthy tendons. Key strategies are thought to include:
- Stretching and Strengthening Exercises: Regularly stretch the calf muscles and Achilles tendon and incorporate exercises to strengthen them, such as heel raises.
- Gradual Warm-Up: Always warm up before engaging in physical activities to prepare the muscles and tendons for exertion.
- Proper Footwear: Wear well-fitted shoes with appropriate support for your activity to minimise strain on the Achilles tendon.
- Avoid Overtraining: Ensure you give your body adequate rest between workouts to prevent overuse injuries.
- Modify High-Risk Activities: If you are at high risk, reduce your participation in sudden bursts of movement, jumping, or abrupt stops.
- Address Underlying Conditions: Manage chronic conditions like diabetes or arthritis that could weaken the tendon.
- Avoid Risky Medications: If you are prescribed medications that might weaken tendons, such as corticosteroids or fluoroquinolones, discuss alternatives with your doctor.
Types of Achilles Rupture
Achilles tendon ruptures can be classified based on the location and severity of the injury:
- Complete Rupture: This is the most severe form of tendon rupture, in which the tendon is completely torn and separates into two sections. It usually requires surgical repair.
- Partial Rupture occurs when only part of the tendon is torn. This results in less dramatic symptoms but still requires medical attention.
- Acute Rupture: A sudden tear caused by a specific event, such as a traumatic injury or abrupt movement.
- Acute on chronic Rupture: The tendon gradually degenerates and weakens, leading to a rupture. It often occurs in individuals with untreated tendinitis or repetitive stress injuries.
- Chronic Rupture: When the tendon has been ruptured and not treated for over 6-12 weeks
- Insertional rupture occurs at the point where the tendon attaches to the heel bone (calcaneus). It is less common but can complicate treatment due to the bone's involvement.
- Mid-substance rupture: The tear occurs in the middle portion of the tendon, which is the most common site due to the reduced blood supply in this area.
Stages of an Achilles Rupture
Achilles tendon ruptures can heal without surgery if the foot is placed in a pointed-down position to bring the tendon ends together. When treated in this way, Achilles tendon rupture typically progresses through the following stages:
- Initial Injury: A sudden, forceful event causes the tendon to tear, leading to sharp pain, a snapping sensation, and immediate difficulty walking or running.
- Acute Inflammatory Phase (First 3-7 Days): The body initiates an inflammatory response. Pain, swelling, and bruising appear around the site of injury. The area becomes tender, and movement is severely limited.
- Subacute Repair Phase (2-6 Weeks): The body begins repairing the tendon by forming scar tissue. Swelling may reduce, but the tendon remains weak and vulnerable to further injury.
- Remodeling Phase (6 Weeks to Several Months): The scar tissue matures, and the tendon regains strength and flexibility. Rehabilitation exercises become critical during this phase to restore function.
- Chronic Phase (Beyond 6 Months): Pain, stiffness, and weakness may persist if healing is incomplete or poorly managed. If untreated, this phase is marked by long-term functional limitations.
Diagnosis of an Achilles Rupture
Diagnosis typically involves reviewing the patient’s history and clinical examination of the tendon. A gap in the tendon can often be felt. An ultrasound or MRI may be ordered to confirm the diagnosis.
Management and Treatment of an Achilles Rupture
The rupture of the Achilles tendon can be managed with or without surgery. Pros and cons include:
- Surgery has a lower re-rupture rate (5-30% lower than no surgery management) and a faster return to normal activity
- Surgery has a higher rate of complications, such as reaction to the anaesthetic, bleeding, wound problems, and infection. An infection can be catastrophic in this area, but luckily, the risk of infection is low at 1-4%.
See Achilles Repair in the Surgery Information section of the website.
Rupture of the Achilles tendon can be managed without surgery as long as:
- The foot is placed into a pointed down position (equinus) within 48 hours
- You are non-weight bearing from the time of the injury
Below are the outlined management and rehabilitation plans with Dr. Graff. All patients are different, and these timelines are only a guide. Some patients may progress faster or slower than others.
0-2 weeks
- You will be in a boot with three wedges or a back slab to keep the foot pointed down for 2-3 weeks
- You can only touch your foot to the ground for balance.
- You will need to bag the leg for showers
- Pain relief: Regular Paracetamol with meals and before bed
- Blood thinning medications for 8 weeks
3-6 weeks
- Start partial weight-bearing in the boot with wedges at 3 weeks; 20% of body weight
- This can increase to 100% of body weight at 6 weeks
- Active range of motion can be performed with the foot pointing down with physio
6-9 weeks
- At 6 weeks, remove one wedge
- At 7 weeks, remove one wedge
- At 8 weeks, remove one wedge
- Continue 100% weight bearing in the boot
- Exercise hip and knee with the boot on
- The boot can be removed for the range of motion of the ankle to neutral with physio
- Isometric calf strengthening with physio
10-12 weeks
- Wean out of the boot at 10 weeks into sneakers
- Always wear shoes even inside
- Increasing strengthening with physio using Theraband for a resisted range of motion of the ankle to neutral
- You can start driving a car
3-6 months
- Avoid lunges/squats or any painful exercises
- Double heel raises as tolerated
- Balance and proprioception with a wobble board
- Standing work is tolerated
6-12 months
- Graduated increase in activity as guided by pain and physio
- Sports-specific training can start
- Jogging stationary bike and single-heel raise
12+ months
- Return to sport when leg feels the same as the unaffected leg in range of movement and strength
What if an Achilles Rupture is Untreated?
Leaving an Achilles tendon rupture untreated can lead to significant long-term complications:
- Chronic Weakness
- Altered Gait and Posture
- Persistent Pain and Swelling
- Tendon Deformity
- Increased Risk of Re-Injury to the limb
Prompt medical intervention and a structured treatment plan are crucial to prevent these complications and ensure optimal recovery.
