Cavovarus Foot
What is Cavovarus Foot Deformity?
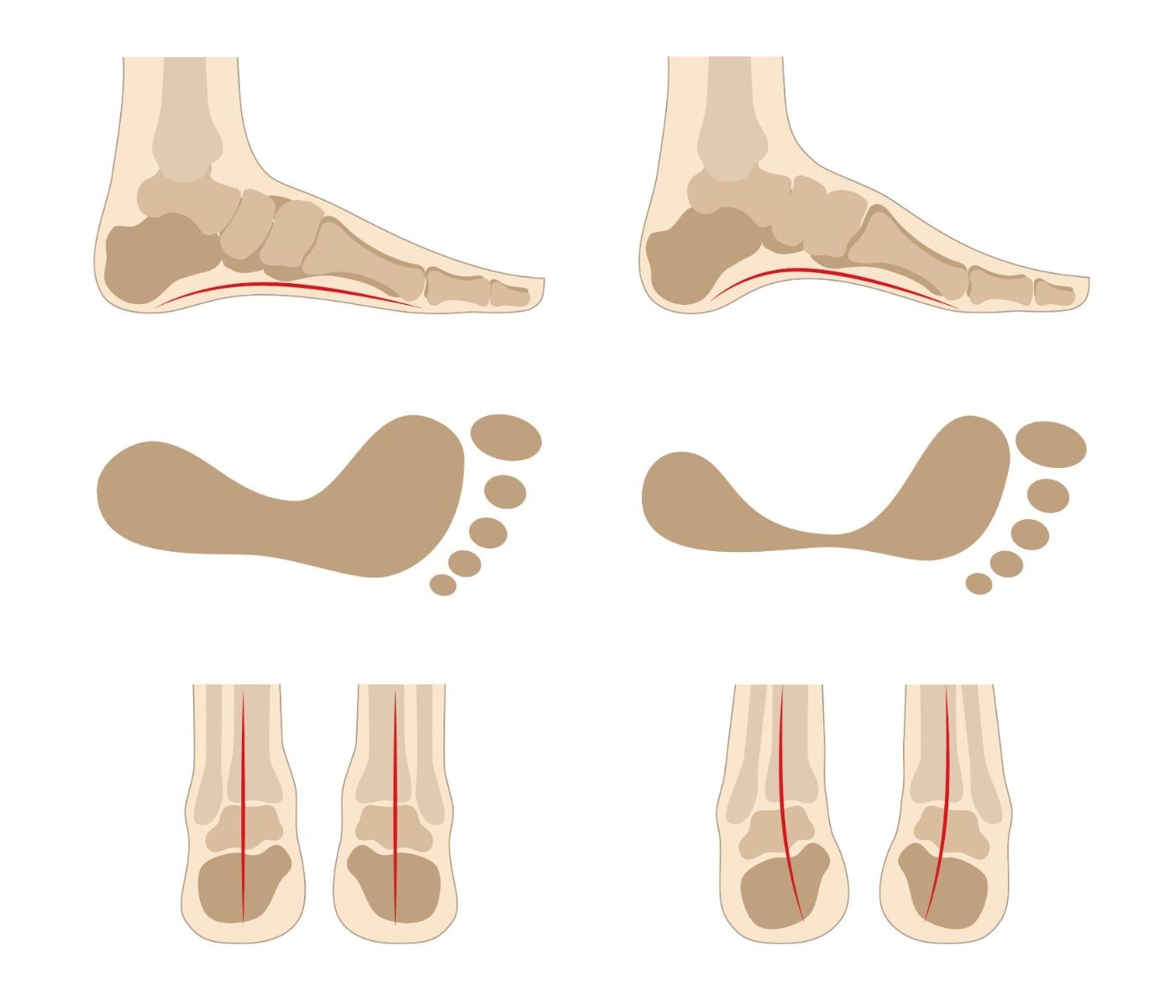
Cavovarus foot is a foot deformity characterised by a high arch and a turned-in heel. It can lead to difficulty walking, pain, and instability. The condition is caused by abnormal foot mechanics, which can be present from birth or develop over time.

Impact of Cavovarus Foot Impact on Anatomy and Health
Cavovarus foot alters the biomechanics of the lower extremities, potentially leading to the following:
- Increased Pressure: Excessive stress on the ball and heel of the foot, leading to calluses and discomfort.
- Instability: Difficulty maintaining balance due to the inward-turned heel, increasing the risk of recurrent ankle sprains.
- Pain: Chronic foot pain, particularly in the arch and heel, due to misalignment and overuse.
- Joint Issues: Over time, the misalignment can lead to arthritis in the foot and ankle.
- Mobility Challenges: Walking and running may become difficult, particularly on uneven surfaces.
Risk Factors for Cavovarus Foot
Many factors, including genetics, nerve or muscle disorders, and trauma to the foot, can cause Cavovarus foot. People with certain medical conditions such as cerebral palsy, clubfoot, muscular dystrophy, or Charcot-Marie-Tooth disease are at an increased risk of developing cavovarus foot. Certain types of foot injuries can lead to the development of this condition.
Causes of Cavovarus Foot
Cavovarus foot can result from various causes, including:
- Congenital Factors: Present at birth due to genetic predisposition or developmental abnormalities.
- Neurological Conditions: Diseases that weaken the muscles and disrupt normal foot alignment.
- Trauma: Fractures, ligament injuries, or nerve damage may lead to the development of cavovarus foot.
- Post-surgical Complications: Procedures involving the foot or ankle can occasionally result in altered alignment.
Symptoms of Cavovarus Foot
- Difficulty walking
- Pain or discomfort in the foot or ankle
- Instability or clumsiness while walking
- Recurrent ankle sprains
- Calluses or corns on the foot
- Deformed or twisted appearance of the foot in severe cases
- Difficulty fitting into shoes
Prevention of Cavovarus Foot
While some cases cannot be fully prevented due to genetic or neurological factors, the following strategies can reduce the risk of severity:
- Early Detection: Regular check-ups for individuals with a family history or known risk factors.
- Supportive Footwear: Shoes with proper support and cushioning can help with symptoms
- Orthotics: Custom insoles can correct minor abnormalities and relieve pressure points.
- Strengthening Exercises: Targeted physical therapy to strengthen foot and ankle muscles.
- Injury Prevention: Use proper techniques and protective gear during sports or physical activities.
- Prompt Treatment: Address foot injuries early to prevent long-term complications.
Types of Cavovarus Foot
Cavovarus foot can be classified into types based on its underlying cause and structural involvement:
- Congenital Cavovarus Foot: Present at birth and often linked to hereditary conditions or developmental abnormalities.
- Neuromuscular Cavovarus Foot: Associated with neuromuscular disorders such as Charcot-Marie-Tooth disease, polio, cerebral palsy or spina bifida.
- Traumatic Cavovarus Foot: Results from injuries to the foot or ankle, including fractures, ligament damage, or nerve trauma.
- Idiopathic Cavovarus Foot: Develops without a clear underlying cause and may be linked to genetic predisposition.
- Post-surgical Cavovarus Foot: Occurs as a previous foot or ankle surgery complication.
Stages of Cavovarus Foot
Cavovarus foot can progress through the following stages:
- Mild Stage: Minimal symptoms and structural changes. The condition may be noticeable but not significantly impairing mobility. The deformity is usually flexible.
- Moderate Stage: Increasing pain, difficulty walking, and visible deformities. Calluses and instability are more pronounced. The deformity is getting stiffer.
- Severe Stage: Advanced structural deformities, chronic pain, and significant mobility impairment. Arthritis and joint damage may develop. The deformity is fixed.
Diagnosis of Cavovarus Foot
Dr Graff will take a history and examine your foot. She will likely arrange imaging, such as X-rays and, in some cases, CT scans or MRIs, to help evaluate the foot's structure. Diagnosing the cause is very important. If the underlying cause is unclear, this may require brain and spine imaging and referral to a neurologist for nerve tests.
Treatment of Cavovarus Foot
Treatment will depend on the severity of the condition and your symptoms. Non-surgical treatments may include custom orthotics, physiotherapy or wearing special shoes. In some cases, surgery may be necessary to correct the foot deformity. Surgical options may include tendon transfers, bone cuts (osteotomy), or rarely joint fusion.
It is important to seek medical review if you suspect you may have cavovarus foot, as early diagnosis and treatment can improve outcomes and quality of life.
Contact Us
If you want more information or have any questions or problems, please contact Dr Graff at admin@christygraff.com or call the rooms at 0493 461 133.
What if Cavovarus Foot is Untreated?
If left untreated, cavovarus foot can lead to:
- Chronic Pain: Persistent foot, ankle, and lower leg discomfort.
- Frequent Injuries: Increased risk of sprains, fractures, and ligament tears.
- Progressive Deformity: Worsening structural misalignment and functional impairment.
- Arthritis: Joint damage and inflammation, particularly in the foot and ankle.
- Reduced Mobility: Difficulty walking, performing daily activities, or engaging in physical activities.
- Skin Complications: Development of ulcers or infections due to abnormal pressure distribution.
Prompt diagnosis and tailored treatment are essential to prevent these complications and improve quality of life.
Useful Websites
