Circular Frame
What is a Circular Frame?
Orthopaedic surgery often involves aligning the bones correctly and using something to hold them in place while the bones heal in the correct position (e.g., plaster, splints, internal fixation, and/or external fixation).
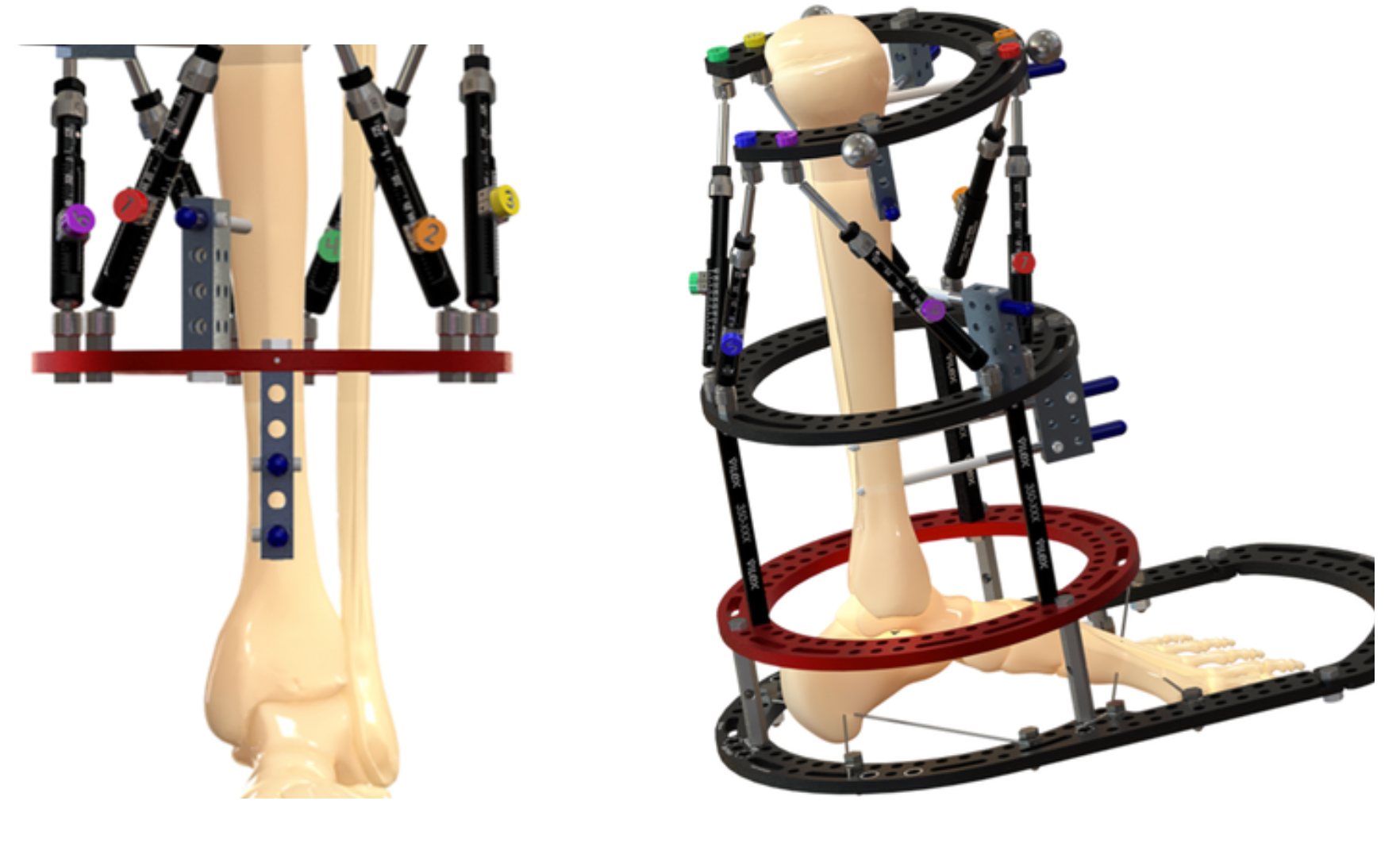
An external fixator is a device on the outside of the skin that holds bone/s in a desired position. A circular frame is a specialised type of external fixator that surrounds a limb and is secured to the bone using wires or pins.
Each frame is individually designed for each patient and depends on the treatment's aim, such as correcting limb deformities, lengthening limbs, healing fractures, or fusion joints.
Who is Suitable for a Circular Frame?
Dr Graff will discuss why a circular frame may be the best treatment.
The most common conditions that require a frame are:
- Lengthening a short limb or correcting a bony deformity
- A fracture which has not healed or has healed in an unacceptable way
- A limb or foot and ankle deformity
- Osteomyelitis (bone infection)
- Complex fractures, including open fractures
- Conditions with poor healing potential of soft tissues
Benefits of a Circular Frame
Walking
Weight-bearing improves bone and muscle strength, joint movement, independence, and confidence. Circular frames often allow weight-bearing through the operated leg while maintaining bone alignment as it heals. Other fixation devices may not be stable enough to allow this. To safely put weight on the foot, you may need a temporary post-operative shoe that fits securely around the frame.
Soft tissue protection
Circular frames allow the surgeon to use smaller incisions to correct major bony problems, with less risk of wound breakdown than a larger incision. Larger incisions that do not heal well can have complications, including infection, multiple surgeries and, in extreme cases, amputation.
Infection prevention
Large wounds often need to be inserted into the internal metalwork. Internal metalwork can act as a place for infection in soft tissue with poor blood supply. Circular frames often have issues with pin site infections, but when treated early, these are usually restricted to the skin. If the infection is more severe, pins may need to be removed.
Gradual distraction/lengthening/correction of the limb or foot
Circular frames often include lengthening by gradual distraction. This allows the body to generate new bone in the space created by the lengthening (1mm per day).
Gradual deformity correction and lengthening are beneficial. It ensures gradual lengthening of the nerves and blood vessels, which reduces the risk of stretching them too quickly. This would otherwise result in ongoing damage and poor function.
Types of Circular Frames
There are several types of circular frames, each designed for specific clinical applications:
- Ilizarov Frame:
- The original circular external fixation device.
- Used for bone lengthening, deformity correction, and fracture stabilisation.
- Taylor Spatial Frame (TSF):
- A more advanced version of the Ilizarov frame.
- Includes computer software for precise multi-dimensional adjustments, making it ideal for complex deformities.
- Hexapod Frames:
- Similar to the Taylor Spatial Frame but with alternative designs and adjustment mechanisms.
- Used for dynamic and accurate correction of bone alignment.
- Hybrid Frames:
- Combines circular rings with other fixation methods, such as half-pins or plates.
- Useful for treating fractures near joints or areas with limited space.
- Rail frames: Linear external fixation, often used in the foot
Alternative Options to Circular Frame
There are usually other options for managing your condition.
Dr Graff will discuss other surgical options, which may include internal fixation (plates and screws or rods under the skin and muscle). Some conditions with limb length discrepancies can be managed with other surgeries, such as shortening the longer leg, timing stopping growth in the longer leg to equalise leg lengths or amputating the shorter leg if there are severe problems. If you have questions about this, please write them down to discuss at your next appointment.
Who looks after the circular frame?
You and your family are the main people who will care for the frame. While in the hospital, the medical and nursing staff will teach you how to care for the pin sites, make adjustments, and tighten any loose parts. Although this may seem daunting, most patients manage very well with the frame at home. Dr Graff works with Noelle Coleman, a nurse practitioner who works via telehealth to support you with your frame. Noelle will educate you and troubleshoot regarding the frame and is an invaluable support.
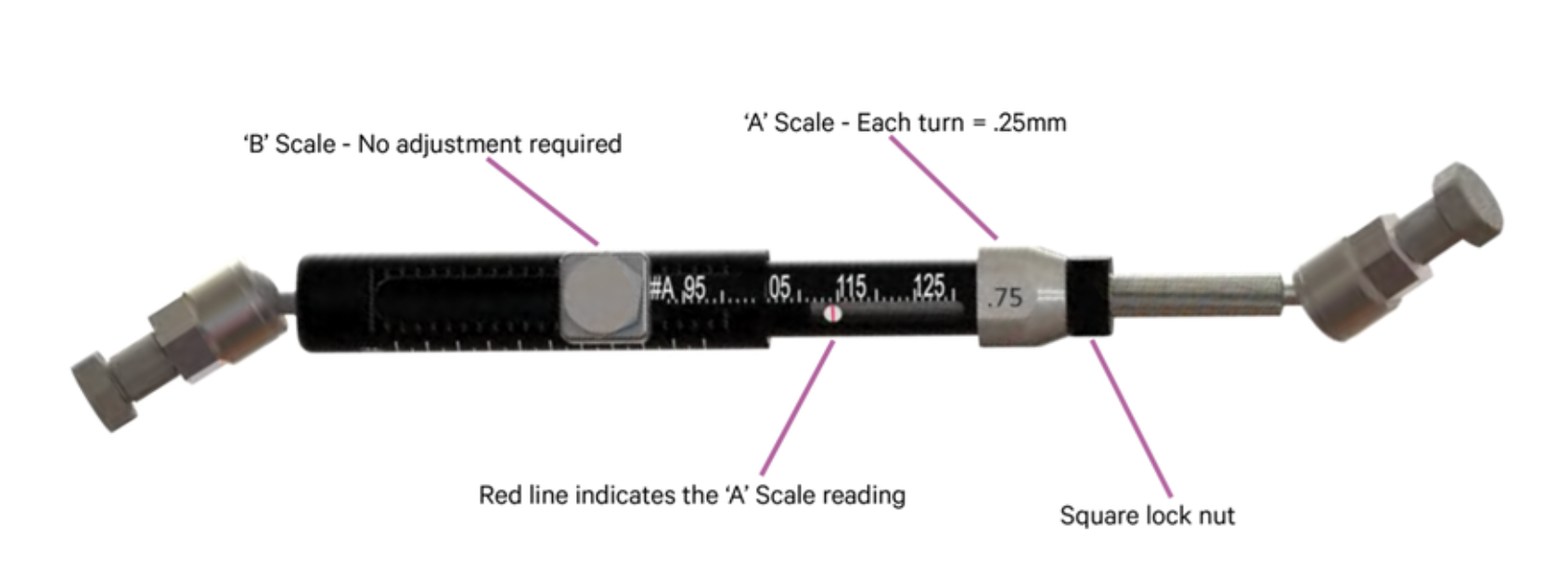
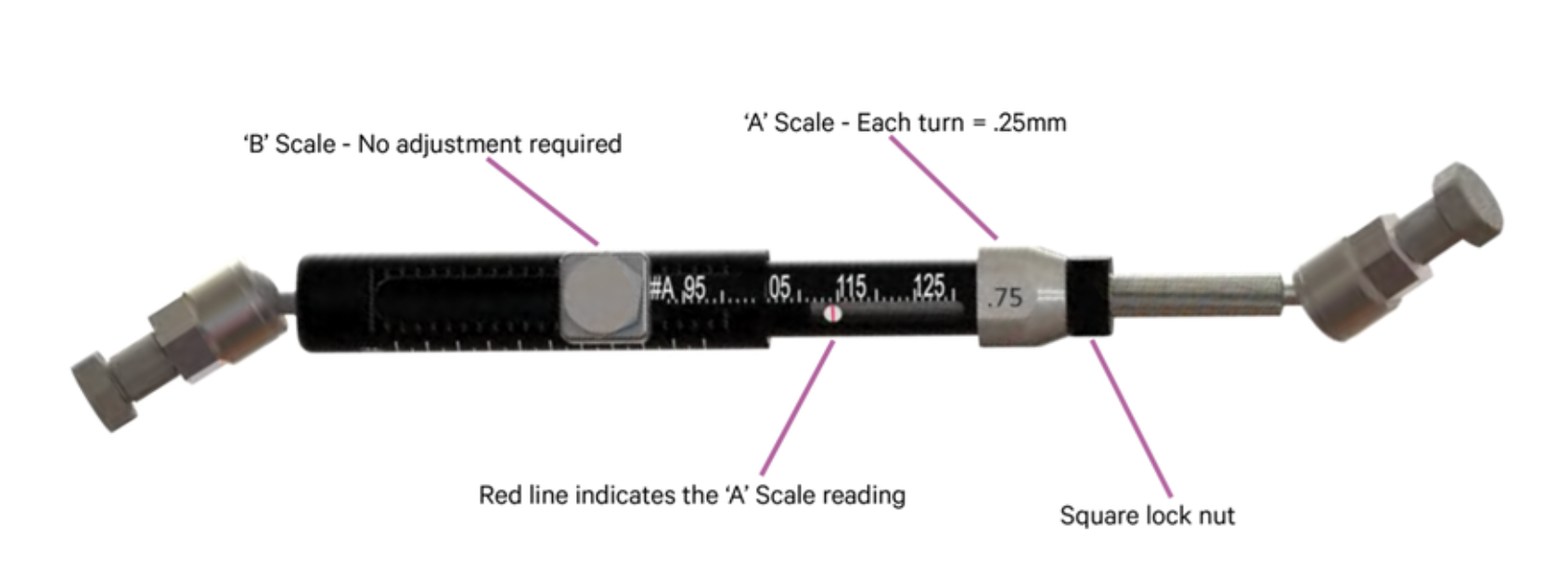
Below is an example of a strut. Dr Graff and/or Noelle Coleman will explain how to use these to make adjustments and ensure they are done correctly.
Prevention of Bunions
While not all bunions can be prevented, certain strategies can reduce your risk:
- Wear Proper Footwear: To minimise stress on the toes, choose shoes with a wide toe box, low heels, and good arch support.
- Maintain a Healthy Weight: Keeping a healthy body weight reduces pressure on the feet and helps prevent joint misalignment.
- Strengthen Foot Muscles: Perform toe stretches and foot rolls to enhance flexibility and muscle strength.
- Use Orthotics: Custom shoe inserts can help improve foot alignment and distribute weight evenly.
- Avoid High Heels: Limit high-heeled or narrow-toed shoes that push the toes out of alignment.
Types of Bunions
Bunions can be classified into different types based on their location and underlying causes:
- Hallux Valgus (Traditional Bunion): The most common type, forming at the base of the big toe. It occurs when the big toe deviates toward the second toe, causing a bony bump on the side of the foot.
- Bunionette (Tailor’s Bunion): A smaller bunion that develops at the base of the little toe. It is often caused by similar factors as traditional bunions, including ill-fitting footwear.
- Adolescent Bunion: Seen in teenagers, especially girls, and often linked to inherited foot structure. These bunions are typically less painful but can worsen over time.
- Arthritic Bunion: Associated with conditions like rheumatoid arthritis or gout, leading to joint swelling and deformity.
- Congenital Bunion: Present at birth, caused by foot structure or alignment abnormalities.
Stages of Bunions
Bunions progress in stages, each with varying levels of severity:
- Mild: Minimal deformity with a slight protrusion at the base of the big toe.
- Moderate: Increased misalignment of the big toe, leading to noticeable swelling and pain.
- Severe: Significant deformity, with the big toe crossing over or under the adjacent toes.
- Complications: Untreated bunions can lead to secondary conditions such as arthritis, corns, calluses, and nerve irritation.
Diagnosis of Bunions
Dr Graff will examine your foot and organise imaging, such as:
- X-rays: To evaluate the bone structure and determine the severity.
- MRI Scans:
Very rarely, but they may be used to view soft tissue and other surrounding structures.
How long is the frame on for?
This depends on why the frame is being used. An average length of time for a circular frame is between 3-6 months.
Circular Frame Journey
Admission
The stay lasts 5-7 days, including rest, recovery, pain relief, rehabilitation, and education. The time spent in the operating suite is generally 2-6 hours.
Pain Relief
Once over the acute post period, frames are not painful but uncomfortable and inconvenient. The fracture and or osteotomy is often the most painful part of the surgery. The pain decreases as it heals. Ultimately, you will need simple pain relief medicine.
If you experience new pain, numbness, or tingling in your limb, contact Dr Graff or present to the Emergency Department for review.
Physiotherapy
Joint contractures are a serious complication of frames. After surgery, a physiotherapist will see you to begin gentle stretches and a range of movement. In the first few days, the aim is to get out of bed. It is important to continue physiotherapy at home, doing joint exercises at least thrice daily.
Frame patients often develop joint stiffness and contractures during treatment, which are difficult to treat once they have developed. It is better to try to prevent this with daily exercises during treatment and regular physiotherapy appointments. You will also be given exercises to do at home.
Wound Care/Showering
Once the surgery wounds have healed (usually 2-3 weeks), daily showers are encouraged to help with pin site care. Dr Graff will inform you when this can start (often after 2-3 weeks post-op). A shower seat might be helpful, as the frame can be heavy and awkward to stand in. Baths are also allowed in clean water.
Pin site care and infection management
During surgery, bandages and extra padding are added to the pin sites to protect them. These bandages will be removed before going home, usually at 10 days. The pin sites are only to be touched if they need cleaning. After the pin site dressings are removed at the two-week appointment, daily showering is usually enough to keep the pin sites clean. Further pin site care is only required if this is not possible or there is concern about an infection.
Hygiene and Skin Care
After surgery, your clothing may need to be bigger than usual to fit around the frame. The frame may catch on clothes, bedding, soft furnishings, and car seats. A pillow between the legs at nighttime can be helpful. Clothes often need to be modified to fit over the external fixator, and examples can be shown to you before surgery.
Suggestions for clothes include:
- Pull away tracksuit pants with Velcro or press studs down the outside seam
- Underwear or boxer shorts can be worn with press studs or velcro down the seam
- Women often find wearing a long skirt a comfortable alternative to pants.
- Patients with a fixator on the upper leg can wear their usual flat shoes.
- A splint may also be necessary to keep the ankle 90 degrees to the leg.
- It may be helpful to have these options ready before surgery so that they can be worn on the ward.

Sleeping
The circular frame may catch and tear bedsheets or cause scratches to your other leg at night. It is recommended to:
- Buy some cheap bedsheets as they tend to get damaged.
- Strap or tie a pillow to the other leg at night for protection
Managing at home
Most patients will spend some time in a wheelchair but should be able to get up using crutches or a frame if possible. This helps rehabilitate muscles, joints, and bones and expedites independence. Please consider whether your house is wheelchair-compatible and whether you need help getting to and from the toilet.
Swimming
Swimming in clean water is encouraged, but beach swimming is not recommended, as sand may get around the pin sites and the frame. If you are swimming, please remember that the external frame is heavy. Please ensure you can safely touch the ground when swimming and/or have someone else around. Swimming does not harm the frame and is excellent exercise and rehabilitation for the limb. You may also be able to participate in hydrotherapy (water therapy) as part of your rehabilitation process.
Circular Frame Risks
Pin site infection
Unfortunately, most people with a circular frame get at least one pin site infection. Dr. Graff will discuss with you the option of staying on oral antibiotics for the frame's duration. Pin site infections can range from redness around a pin site, which responds to oral antibiotics at home, to more serious infections, which may require hospital admission, intravenous antibiotics, and even a trip to the theatre to remove the pin. If you suspect you have a pin site infection, contact Dr Graff or Noelle or present it to your local Emergency Department for a review.
Joint contractures/dislocations
Joint contractures or stiffness (i.e. of the hip, knee and ankle) can be major problems during and after a frame. You need to get used to moving your joints from the day after surgery. If gradual correction occurs, joint stiffness can worsen as correction continues. This is because the muscles, tendons, ligaments and other soft tissues that cross the joint are being stretched, which can cause the joint to become more difficult to move. You need to engage in physiotherapy both at home and at appointments.
Nerve changes
Even if nerves are getting stretched gradually, they can still become unhappy and cause discomfort, altered sensation or loss of function. Occasionally, this can be permanent. If you experience new numbness, tingling or pain in any part of your limb, present it to the Emergency Department for a review or call Dr Graff or Noelle. To prevent permanent nerve damage, it may be that the corrections or lengthening need to be paused, stopped, or even reversed. Itching or nerve sensitivities may be addressed with medication.
Returning to surgery
Everyone with a circular frame will need another operation; some patients may need two or three more. Common reasons for this include frame adjustment, removal of infected pins, removal of the frame, or nerve or joint releases. These surgeries are often much smaller than the original surgery, and patients can usually go home the same day.
Home Care and Follow-up
Important Considerations
One or more family members must stay at home for several weeks while you recover or undergo rehab. Please consider this when considering this surgical option. You may take time to regain your independence in terms of hygiene and getting around the house. You must attend multiple outpatient appointments in the first few weeks, often weekly or fortnightly.
Appointments
You will be seen regularly during the correcting/lengthening of the frame (often weekly). X-rays are often done at these appointments. Some of these appointments may be able to be done via telehealth if you don’t live locally. This can be discussed with Dr Graff.
Circular Frame Prognosis
The prognosis for patients with a circular frame is generally positive, especially those with complex bone conditions.
Circular frames effectively treat fractures, deformities, and limb length discrepancies, with high rates of successful outcomes. Patients typically see gradual correction of deformities or bone healing over weeks to months, depending on the case's complexity.
With proper rehabilitation, most patients regain good function of the affected limb. Bone strength and alignment are often restored to near-normal levels.
What if a Circular Frame is Delayed?
Delaying the application of a circular frame can have significant consequences, depending on the underlying condition:
- Worsening of the Condition
- Increased Risk of Complications
- Prolonged Pain and Discomfort
- More Invasive Treatment Required
- Emotional and Psychological Impact
In most cases, delaying treatment with a circular frame is not advisable, as early intervention leads to better outcomes and fewer complications.
