Insertional Achilles Tendinopathy Surgery
What is Insertional Achilles Tendinopathy Surgery?
Insertional Achilles Tendinopathy Surgery is a procedure designed to treat chronic pain and inflammation at the point where the Achilles tendon inserts into the heel bone (calcaneus). This condition occurs when the tendon degenerates or inflates due to overuse, wear and tear, or structural issues.
Who is Suitable for Insertional Achilles Tendinopathy Surgery?
Patients who are ideal candidates for this surgery typically meet the following criteria:
- Persistent Pain: Severe pain and stiffness in the back of the heel that interferes with daily activities or exercise.
- Failed Non-Surgical Treatments: Lack of improvement after trying conservative methods like rest, physiotherapy, podiatry, corticosteroid injections, or shockwave therapy.
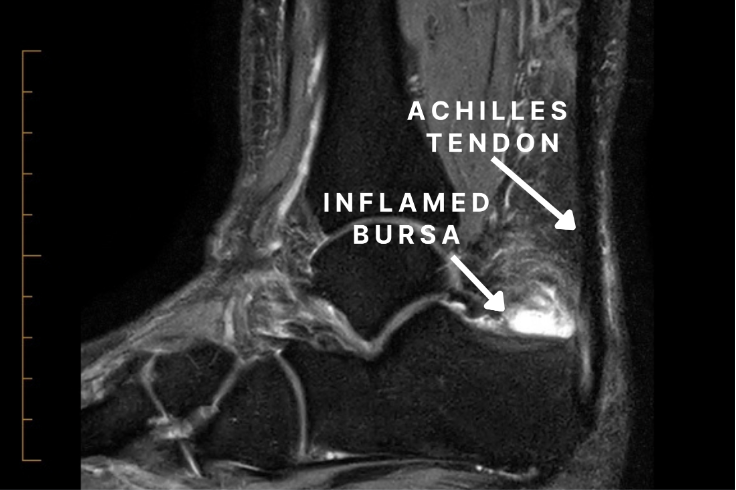
- Degenerative Changes: Confirmed damage to the tendon or calcaneal bone spurs, often diagnosed via imaging (e.g., MRI)).
- Activity Limitations: Significant mobility, walking, or running limitations due to the condition.
- Good Overall Health: The patient should be fit for surgery with no severe underlying conditions that could impair healing.
Benefits of Insertional Achilles Tendinopathy Surgery?
The potential benefits of this surgery include:
- Pain Relief: Significant reduction or elimination of chronic pain in the heel and Achilles tendon area.
- Improved Mobility: Enhanced range of motion and function, enabling patients to walk, run, or engage in physical activities without discomfort.
- Restored Tendon Strength: Repaired and reinforced tendons to support regular activity and reduce the risk of future injuries.
- Improved Quality of Life: Relief from chronic pain often leads to better overall mental and physical well-being.
- Addressing Underlying Issues: Removal of bone spurs and damaged tissue prevents further degeneration and complications.
Types of Insertional Achilles Tendinopathy Surgery
The types of surgery depend on the severity and specific nature of the condition:
- Debridement and Spur Removal:
- Removal of degenerated tendon tissue and calcifications or bone spurs at the insertion point.
- Best suited for mild to moderate cases.
- Tendon Transfer:
- Used when a significant portion of the tendon is damaged or degenerated.
- Involves transferring a tendon to the big toe to bring blood supply and function to the damaged area of the Achilles tendon
- Calcaneal Osteotomy:
- Reshaping or shaving of the heel bone to reduce irritation to the tendon.
- Typically performed alongside tendon repair.
Alternative Options to Insertional Achilles Tendinopathy Surgery
Before considering surgery, many patients explore non-invasive or minimally invasive treatments, including:
- Physiotherapy: Focused exercises to improve tendon strength and flexibility.
- Orthotics and Footwear Adjustments: Heel lifts or specialised shoes to reduce strain on the Achilles tendon.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) to manage pain and inflammation.
- Shockwave Therapy: Use of high-energy sound waves to stimulate healing and reduce pain.
- Platelet-Rich Plasma (PRP) Injections: Concentrated platelets from the patient’s blood are injected into the affected area to promote healing.
- Lifestyle Modifications: Avoiding activities exacerbating the condition and incorporating low-impact exercises like swimming or cycling.
Preparation Before an Insertional Achilles Tendinopathy Surgery
Preparation for surgery is essential to optimise outcomes and minimise complications. Follow these steps:
- Medical Evaluation: Consult Dr. Graff to confirm the diagnosis and assess its severity. Provide a complete medical history, including medications, allergies, and chronic health conditions.
- Pre-Operative Testing: Imaging tests, such as X-rays, MRI, or ultrasound, may be required to evaluate tendon damage and calcifications.
- Medications: Discuss any medications or supplements you are taking. You may need to stop blood thinners (e.g., aspirin) a few days before surgery.
- Lifestyle Adjustments: Quit smoking, as it can impair healing. Maintain a healthy diet of proteins, vitamins, and minerals to support post-surgery recovery.
- Pre-Surgical Instructions: Avoid eating or drinking for a specified period (usually 8–12 hours) before the procedure. Arrange transportation and support for the recovery period.
- Physiotherapy: Some patients may benefit from pre-surgery exercises to strengthen surrounding muscles and improve flexibility.
Insertional Achilles Tendinopathy Surgery Procedure
- The surgery involves an incision over the Achilles insertion and detachment of the insertion from the bone.
- The bone spur, bursa and degenerative tendon are removed.
- The tendon is then sutured back using bone anchors.
- Sometimes, a tendon transfer is performed to improve strength and blood supply to the repair.
The Hospital Stay
- You wake up with bulky bandages, a boot with 3 wedges inside
- You will stay in the hospital overnight, with your foot elevated, and you will have antibiotics through a drip.
- You will need blood thinners to prevent DVT and vitamin C to help with wound healing and pain management.
- You will be only allowed to touch your foot to the ground for 2-3 weeks
- Depending on your balance and strength, you may need rehabilitation post-operatively
- Buying a second-hand knee scooter pre-operatively (you can search online) and practising at home before the surgery can be helpful; please bring it into the hospital with you. It is easier to use a knee scooter than crutches.
At Home
- You will need medications for pain relief
- You will need blood thinners and vitamin C daily for 6-8 weeks
- Please leave all dressings intact until your appointment with Dr Graff
- You will get an appointment for your post-op appointment in 2-3 weeks, where the dressings will be taken down
- After this, you will be able to shower normally and pat the dressings dry
Insertional Achilles Tendinopathy Surgery Rehabilitation
All patients are different. These timelines are only a guide; some patients may progress faster or slower than others.
0-2 Weeks
- You will be in a boot with 3-4 wedges
- You can only touch your foot to the ground for balance.
- You will need to bag the leg for showers.
- Pain relief: Please take regular paracetamol with meals and before bed; you may need stronger painkillers as well, especially before bed
- Please take blood thinners and vitamin C as prescribed
2-4 Weeks
- Post-op appointment with Dr Graff
- You will then go back into the boot with three wedges to wear at all times except for showering
- You can start partial weight bearing in the boot (20-50% body weight)
- You can take the boot off for showers only to sit on a shower chair and keep the foot pointed down
- You can start physio for isometric calf strengthening, hip and knee strengthening, and leg lifts with the boot on
4-6 Weeks
- You can remove one wedge per week from the boot
- You can increase to full weight bearing in the boot
- You can start active theraband inversion and eversion exercises below neutral with physiotherapy
6-8 Weeks
- Post-op appointment with Dr Graff
- You can weight bear as tolerated in the boot without wedges
- Physiotherapy for active plantarflexion and dorsiflexion to neutral (pain-free) and continue resisted inversion/eversion with a foot in neutral and proprioception training
9-12 Weeks
- You can wear normal shoes if you can fit into them (you may still have swelling)
- You can range the ankle past neutral with physiotherapy
3-6 Months
- Post-op appointment with Dr Graff
- You can progress in strengthening and range of motion with pain-free double leg heel raises with physiotherapy
- From 4 months, light jogging can commence if there is no pain
- You can walk barefooted
6-12 Months
- When the leg feels back to normal and the same as the other leg, you can start sport-specific training and heavy labour work.
When Can I Return To Work/School?
- Seated work 4-6 weeks
- Prolonged standing 10-12 weeks
- Heavy labour work 9-12 months
When Can I Return To Sport?
- Start sport-specific training at 6-8 months.
- Return to sport when the leg is the same as the other side (9-12 months)
When Can I Drive?
- Left foot 4-6 weeks (if driving an automatic)
- Right foot 10-12 weeks
Insertional Achilles Tendinopathy Surgery Prognosis
The prognosis for this surgery is generally positive, with most patients experiencing significant pain relief and improved function. Success rates range from 80% to 90%, depending on factors such as the extent of tendon damage, adherence to rehabilitation, and individual health conditions.
- Short-Term: Pain relief and gradual improvement in mobility.
- Long-Term: Most patients return to regular physical activities, though some may experience mild residual stiffness.
Insertional Achilles Tendinopathy Surgery Risks
As with any surgery, there are potential risks, though complications are uncommon:
- Anaesthetic problems
- Nerve injury
- Blood clots
- Infection
- Stiffness Rupture
- Ongoing pain
- Further surgery
What if Insertional Achilles Tendinopathy Surgery is Delayed?
Delaying surgery can have several implications:
- Progressive Damage: Continued Achilles tendon degeneration leads to more severe pain and mobility limitations.
- Chronic Inflammation: Persistent inflammation can result in scar tissue formation, complicating future treatment.
- Reduced Quality of Life: Pain and limited mobility may interfere with daily activities, work, or exercise.
- Potential Rupture: In severe cases, untreated tendinopathy can lead to an Achilles tendon rupture, requiring more extensive surgery and a longer recovery.
- Increased Surgical Complexity: Advanced damage may necessitate more complex reconstructive procedures and a longer recovery period.
If you want more information or have any questions or problems, please contact Dr Graff at admin@christygraff.com or call the rooms at 0493 461 133.
