Achilles Tendon Repair
What is Achilles Tendon Repair?
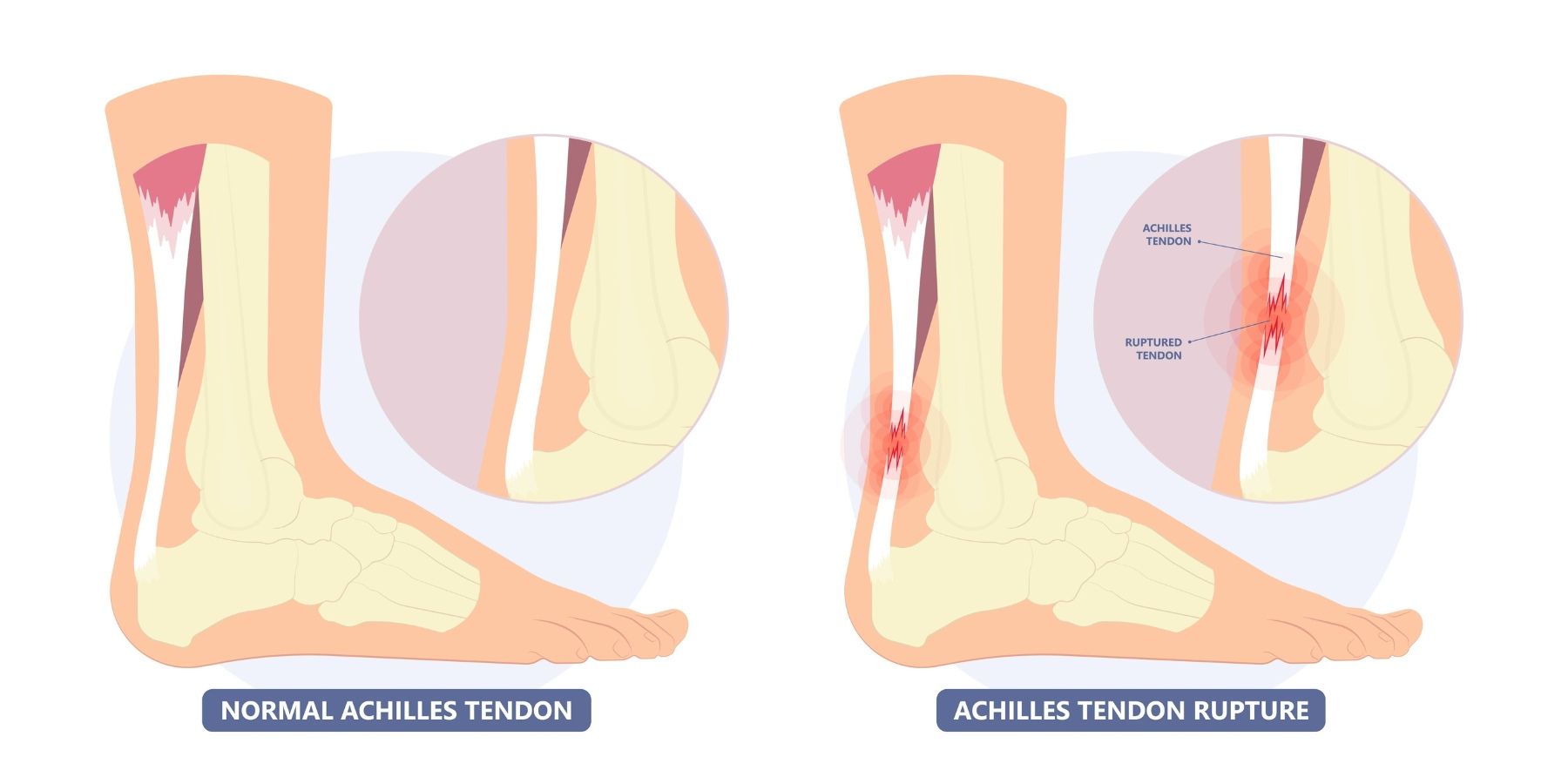
Achilles tendon repair is a surgical procedure to treat a torn or ruptured Achilles tendon, which connects the calf muscles to the heel bone. The procedure aims to restore the tendon’s function and strength, enabling patients to regain mobility. It is often performed when the tendon is severely injured or if non-surgical treatments are insufficient for healing.

Who is Suitable for Achilles Tendon Repair?
Achilles tendon repair is typically suitable for:
- Individuals with a complete Achilles tendon rupture: Those who experience significant pain, swelling, or inability to push off the ground with the affected foot.
- Athletes or active individuals: Especially those needing a faster or more reliable recovery to return to high levels of physical activity.
- Younger or middle-aged patients: Often prioritised for surgical repair due to their higher activity levels and recovery potential.
- Failed non-surgical treatments: Patients whose tendon has not healed properly with conservative methods like bracing or physical therapy.
Benefits of Achilles Tendon Repair
The benefits of Achilles tendon repair include:
- Restoration of tendon strength: Allows normal walking, running, and jumping.
- Improved mobility and flexibility: Helps regain a full range of motion faster.
- Reduced risk of re-injury: Proper repair minimises the chances of future ruptures.
- Faster recovery time for active individuals: Compared to non-surgical methods, surgery allows patients to weight-bear faster and speeds up recovery.
- Enhanced quality of life: Resolves chronic pain and restores functionality for those with chronic tears.
Types of Achilles Tendon Repair
Achilles tendon repair can be categorised into several types based on the technique used:
- Open Surgery: A single incision is made to access and repair the tendon.
- Tendon Transfer: A nearby tendon may be transferred to compensate for the damaged Achilles tendon in chronic tears.
Alternative Options to Achilles Tendon Repair
For patients who may not require or be suitable for surgery, alternative treatments include:
- Non-Surgical Treatments (see Achilles Tendon Rupture Information Sheet):
- Immobilisation: Using a cast or a boot to keep the foot in a pointed down position within the first 48 hours of injury to keep the tendon in a healing position.
Preparation Before an Achilles Tendon Repair
Preparation for Achilles tendon repair involves several steps to ensure a smooth procedure and recovery:
- Consultation with a Specialist:
- Undergo a thorough evaluation by Dr Graff.
- Review imaging tests like MRI or ultrasound to assess the injury.
- Medical Clearance:
- Inform your doctor about any medical conditions, medications, or allergies.
- Stop taking blood-thinning medications (e.g., aspirin) as instructed.
- Lifestyle Adjustments:
- Avoid smoking to promote better healing.
- Maintain a balanced diet to support recovery.
- Pre-Surgery Instructions:
- Fast as directed (typically no food or drink for 8-12 hours before surgery).
- Arrange for transportation and post-operative assistance.
- Rehabilitation Planning:
- Coordinate with a physical therapist to understand the recovery process.
- Prepare your home with necessary aids like crutches or a walker.
Achilles Tendon Repair Procedure
Achilles tendon repair typically follows these steps:
- The surgery involves one long incision over the site of the Achilles tendon.
- The Achilles tendon ends are identified and sutured together.
- The soft tissue tube surrounding the repair (paratenon) is closed over the repair.
- The wound is then closed, and a boot with 3-4 wedges is placed.
The Hospital Stay
- You wake up with bulky bandages and a post-op boot with 3-4 wedges.
- Your foot will be elevated overnight, and you will receive antibiotics through a drip.
- You will need blood thinning medications for 8 weeks
- You will only be able to touch your foot to the ground.
When You Go Home
- You will need medications for pain relief.
- You will need blood-thinning medications to prevent blood clots for 8 weeks.
- You will need to take vitamin C 1g daily for 6 weeks
- Please leave all dressings intact until your appointment with Dr Graff.
- You will get an appointment for your post-op appointment in 2-3 weeks, during which the dressings will be removed.
- After this, you can normally shower on a shower chair and pat the dressings dry, but only if you keep your foot pointed down. You will still need the boot to sleep.
Achilles Tendon Surgery Rehabilitation
All patients are different, and these timelines are only guides; some may progress faster or slower than others.
- You will need a boot with 3-4 wedges for 4 weeks.
- You will have appointments with Dr Graff at 2 weeks and 6 weeks.
0-2 weeks
- You will be in a boot with 3-4 wedges.
- You can only touch your foot to the ground for balance.
- You will need to bag the leg for showers.
- Pain relief: Please take regular Panadol with meals and before bed.
- Please take blood-thinning medications as prescribed and 1g of vitamin C for 6 weeks.
2-4 weeks
- Post-op appointment with Dr Graff.
- You will return to the boot with three wedges for another 1-2 weeks.
- You can start weight bearing in the boot.
- You can take the boot off for showers, sit in a shower chair, and keep the foot pointed down.
- You can start isometric calf strengthening.
- You can start hip and knee ROM strengthening and lifts with the boot on.
4-6 weeks
- You can remove one wedge per week of the boot.
- You can increase active dorsiflexion to neutral with physiotherapy.
- You can start active theraband inversion and eversion exercises below neutral with physio.
- You should continue hip and knee exercises with the boot on. You will then have an appointment with Dr. Graff and an X-ray.
6-8 weeks
- Post-op appointment with Dr Graff.
- You can weightbear as tolerated in the boot without wedges.
- Active plantarflexion and dorsiflexion to neutral (pain-free) and continue resisted inversion/eversion with a foot in neutral.
- Commence proprioception training.
9-12 weeks
- You can wear normal shoes if you fit into them (you may still have swelling).
- You can range the ankle past neutral with physio.
- You can start cycling/swimming.
3-6 months
- Post-op appointment with Dr Graff.
- You can progress strengthening and range of motion with pain-free double-leg heel raises and single-leg balance with physio.
- From 4 months, light jogging can commence if there is no pain.
6-12 months
- When the leg feels back to normal and is the same as the other leg, you can start sport-specific training and heavy labour work.
When Can I Return To Work/School?
- Seated work 4-6 weeks.
- Prolonged standing 10-12 weeks.
- Heavy labour work 9-12 months.
When Can I Return To Sport?
- Start sport-specific training at 6-8 months.
- Return to sport when the leg is the same as the other side (9-12 months).
When Can I Drive?
- Left foot 6-8 weeks.
- Right foot 10-12 weeks.
Achilles Tendon Repair Prognosis
The prognosis for Achilles tendon repair is generally favourable:
- Success Rates: Most patients regain full strength and mobility.
- Recovery Time: Complete healing usually occurs within 6-12 months.
- Long-Term Outcomes: Proper rehabilitation reduces the risk of re-rupture, especially in younger and active individuals.
Achilles Tendon Repair Risks
As with any surgery, Achilles tendon repair carries some risks:
- Anaesthetic problems.
- Nerve injury.
- Blood clots.
- Infection.
- Stiffness.
- Re-rupture.
- Ongoing pain.
- Further surgery.
What if Achilles Tendon Repair is Delayed?
Delaying repair of a torn Achilles tendon can lead to complications, such as:
- Chronic Pain: Persistent discomfort and swelling.
- Reduced Mobility: Difficulty walking, running, or performing daily activities due to lack of push-off.
- Tendon Shortening or Weakness: Making later repairs more complex.
- Muscle Atrophy: Loss of calf muscle strength due to prolonged inactivity.
- Poor Long-Term Outcomes: Increased risk of incomplete recovery or re-rupture.
If repair is delayed, consult an orthopedic specialist immediately to discuss tailored treatment options and rehabilitation plans.
Contact Us
If you want more information or have any questions or problems, please contact Dr Graff at admin@christygraff.com or call the rooms at 0493 461 133.
