Adult Acquired Flat Foot
What is Adult Acquired Flat Foot (AAFF)?
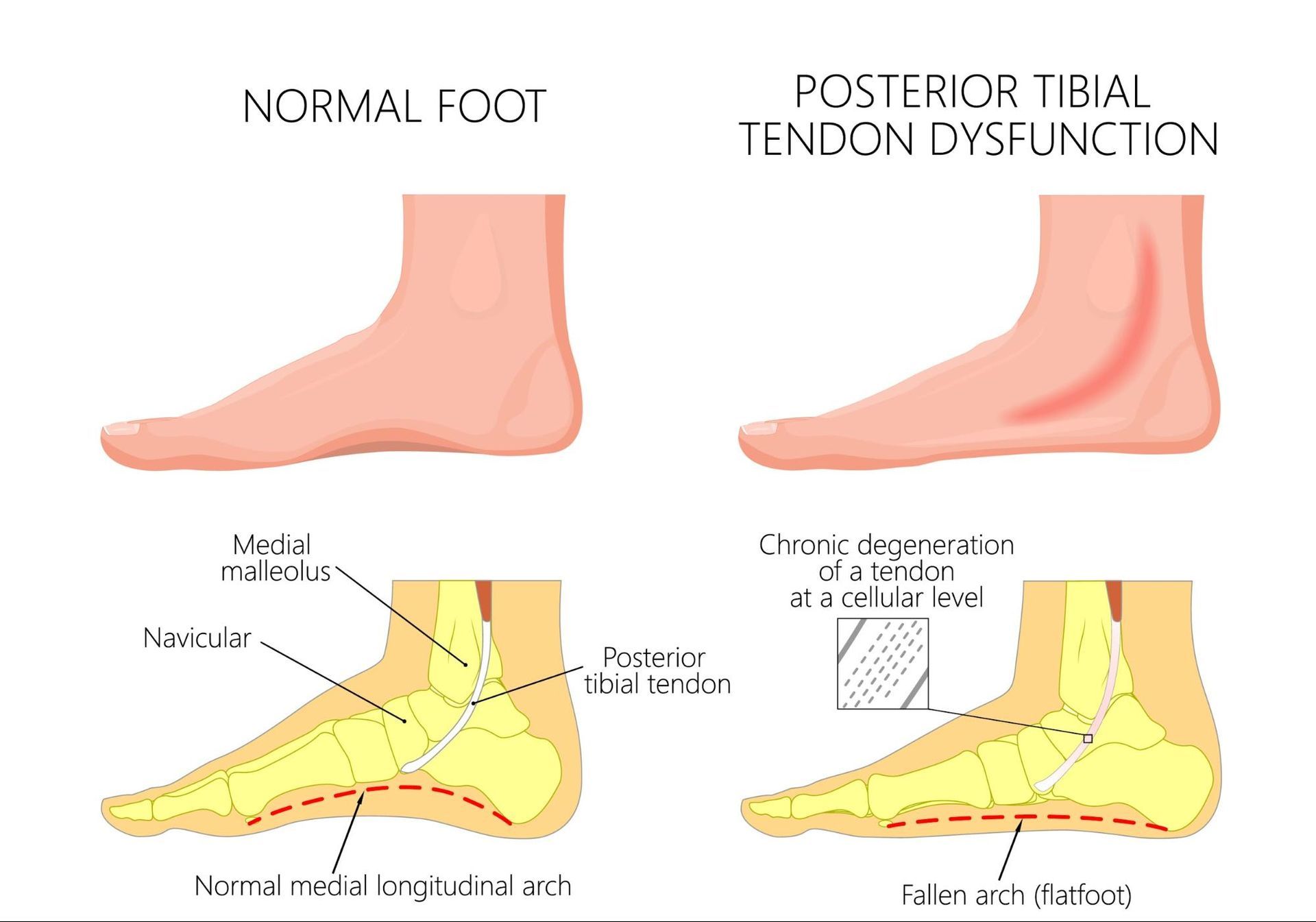
This condition has many names and differs from people who grow up with flat feet. Other names for the condition include tibialis posterior insufficiency or progressive collapsing foot deformity (PCFD). AAFF is a complex deformity in which an important tendon (tibialis posterior) degenerates and can not stabilise the foot arch, which progressively flattens.

Impact of Adult Acquired Flat Foot on Anatomy and Health
Adult Acquired Flat Foot primarily affects the structure and function of the foot and ankle. It can lead to:
- Biomechanical Imbalance: The flattening of the arch alters the alignment of the foot and ankle, causing strain on surrounding joints, tendons, and ligaments.
- Pain and Discomfort: The arch's collapse often results in pain along the inner side of the foot, ankle, or lower leg due to overuse or inflammation of the posterior tibial tendon.
- Reduced Mobility: As the foot loses its natural shock-absorbing capabilities, it may become difficult to walk, stand, or engage in physical activities.
- Secondary Problems: If untreated, AAF can contribute to knee, hip, and lower back pain due to changes in posture and gait.
Risk Factors of Adult Acquired Flat Foot
Several factors increase the risk of developing Adult Acquired Flat Foot, including:
- Previous injury
- Genetics
- Repetitive use of the foot and ankle
- Female
- >40 years old
- Increased weight
- Diabetes
- Rheumatoid arthritis
Causes of Adult Acquired Flat Foot
The tibialis posterior is a big tendon on the inside of the foot. The spring ligament, which helps support the foot arch, is also important. Both can slowly stretch out over time, changing the foot's shape as the structures on the inside stretch out and become flatter.
Symptoms of Adult Acquired Flat Foot
Symptoms of AAF can vary based on the severity and underlying cause, but common signs include:
- Pain on the inside of the foot and ankle
- Pain in the inside of the arch
- Pain and weakness with activity
- Increasing deformity of the foot, with loss of the arch and the foot turning outwards
- Increasing pain on the outside of the foot due to the change of shape of the foot, causing impingement of bones and tendons
Prevention of Adult Acquired Flat Foot
While not all cases of AAFF can be avoided, you can take steps to reduce the risk:
- Maintain a Healthy Weight: Keeping your weight within a healthy range minimises stress on your feet and tendons.
- Wear Proper Footwear: Supportive, well-fitted shoes with arch support can prevent strain on the foot.
- Strengthen Foot Muscles: Regular exercises, such as toe raises and foot stretches, can strengthen the arch and support tendons.
- Avoid Overuse: Rest your feet after prolonged standing or heavy activity periods to prevent overuse injuries.
- Monitor Health Conditions: Manage underlying conditions like arthritis or diabetes that can contribute to tendon problems.
- Seek Early Treatment: Promptly address minor foot or ankle pain to prevent worsening conditions.
Types of Adult Acquired Flat Foot
Adult Acquired Flat Foot can manifest differently depending on the underlying cause and structural changes. The primary types include:
- Posterior Tibial Tendon Dysfunction (PTTD):
- The most common type, caused by repetitive injury or degeneration of the posterior tibial tendon.
- This leads to a gradual arch collapse, inward ankle rolling, and, ultimately, a stiff, misshapen foot.
- Arthritic Flat Foot:
- Occurs due to arthritis, particularly rheumatoid arthritis or osteoarthritis, which damages the joints and ligaments supporting the arch.
- Associated with pain and stiffness in the foot and ankle.
- Traumatic Flat Foot:
- Caused by fractures, dislocations, or other injuries that disrupt the structural integrity of the foot.
- The flattening of the arch occurs rapidly after trauma, such as a Lis Franc injury (see Lis Franc Injury Information sheet).
- Neurological Flat Foot:
- Results from conditions such as cerebral palsy, stroke, peripheral neuropathy, or nerve damage that weaken the muscles supporting the foot.
- Typically associated with other neurological symptoms.
Stages of Adult Acquired Flat Foot
Adult Acquired Flat Foot typically progresses through four stages:
- Stage I: Mild symptoms with inflammation or pain in the posterior tibial tendon. The arch remains intact, which is often reversible with early intervention.
- Stage II: Partial or complete rupture of the posterior tibial tendon, leading to noticeable flattening of the arch. The foot begins to roll inward (pronation), and the deformity remains flexible.
- Stage III: The deformity becomes rigid, with significant arch flattening. Pain and stiffness are prominent, and conservative treatments may be less effective.
- Stage IV: Advanced stage involving ankle joint arthritis. Severe pain, deformity, and disability, often require surgical intervention.
Diagnosis of Adult Acquired Flat Foot
Dr Graff will examine your foot and ankle to assess the tendons and joints in the foot. X-rays are usually taken of both feet while you are standing. An MRI scan can be useful to assess the tendons and ligaments in the foot. Sometimes, weight-bearing CT scans can help with planning the surgery.


Management and Treatment of Adult Acquired Flat Foot
Treatment is aimed at managing the pain and preventing or slowing deformity. Management options include:
- Medications: regular paracetamol and/or ibuprofen with foot can help with pain
- Resting from aggravating activities: Impact activities worsen the symptoms and progression of the deformity and pain
- Weight loss: the more weight that is put through your foot, the worse the pain and progression can be.
- Orthotics and bracing: A brace or orthotic (either from the chemist, orthotist or podiatrist) can help support the foot and ankle to help with the pain. Supportive lace-up boots can also help with pain and support the foot and ankle in the earlier stages.
- Physiotherapy: Strengthening and stretching can help with more mild stages of the disease
- Injections: Ultrasound-guided injections can be diagnostic, i.e. help determine where the pain is, and also can help treat the pain and inflammation
- Surgery: Depending on the underlying cause and problem, various surgeries can help (See Flat Foot Reconstruction Surgery Information Sheet).
Surgery would be tailored to the stage of AAFF and the symptoms. If you want an opinion on this condition, please book an appointment with Dr Christy Graff here.
What if Adult Acquired Flat Foot is Untreated?
If left untreated, AAF can lead to significant complications, including:
- Persistent pain due to ongoing inflammation, joint damage, and strain on the surrounding tissues.
- Progression to a rigid deformity that becomes harder to treat and impacts mobility.
- Knee, hip, and lower back problems due to altered gait and posture.
- Difficulty performing daily activities, walking, or wearing normal footwear.
- Accelerated development of arthritis in the foot and ankle joints.
- Increased risk of disability
Early diagnosis and treatment are critical to managing Adult Acquired Flat Foot and preventing complications.
