Insertional Achilles Tendinopathy
What Is Insertional Achilles Tendinopathy (IAT)?
The Achilles tendon is the large tendon at the back of the heel. It is important for walking. Insertional Achilles tendinopathy occurs as we get older with ‘wear and tear’ and overuse. Over time, the tendon becomes drier and scarred, leading to tears and inflammation. A bone spur can develop over time and cause rubbing and more pain. Rupture (complete tear) of the tendon can occur in severe cases.
Impact of Insertional Achilles Tendinopathy on Anatomy and Health
IAT directly affects the structural integrity of the Achilles tendon and its connection to the heel. Over time, repetitive stress or degeneration can lead to microtears, swelling, and damage to the surrounding tissues. Some common anatomical and health impacts include:
- Reduced Flexibility: Tightness in the tendon or surrounding muscles may limit ankle mobility.
- Pain and Swelling: Persistent pain at the back of the heel can interfere with daily activities and sleep.
- Calcification: Chronic cases may lead to bony growths (bone spurs) where the tendon inserts into the heel.
- Activity Limitation: Routine activities such as walking or climbing stairs can become difficult.
- Muscle Weakness: Prolonged disuse or reduced activity levels can weaken the calf muscles and tendons.
Risk Factors for Insertional Achilles Tendinopathy
Certain factors may increase the risk of insertional Achilles tendinopathy, such as:
- Age over 35 years old
- Overuse, repetitive use or increased use
- High body weight
- Ankle tendon stiffness
Causes of Insertional Achilles Tendinopathy
Insertional Achilles tendinopathy can arise from a variety of factors:
- Overuse or Repetitive Stress: Frequent high-impact activities like running or jumping can overload the tendon.
- Sudden Increase in Activity Levels: Quickly ramping up exercise intensity or frequency without preparation can strain the tendon.
- Tight Calf Muscles: Limited flexibility in the calf muscles increases tension in the Achilles tendon.
- Aging and Degeneration: Natural wear and tear over time can weaken tendon fibres.
- Biomechanical Issues: Poor foot alignment or gait mechanics can contribute to increased stress at the tendon insertion site.
Symptoms of Insertional Achilles Tendinopathy
Insertional Achilles tendinopathy typically presents with the following symptoms:
- Pain, a burning feeling and/or swelling at the back of the heel
- Tenderness to touch at the back of the heel
- Difficulty with rubbing of shoes
- Symptoms tend to be worse at the beginning or end of the day
- Weakness of push-off at the ankle
Prevention of Insertional Achilles Tendinopathy
Although not all cases of IAT can be prevented, adopting certain strategies can significantly reduce the risk:
- Stretch Regularly: Incorporate calf and Achilles tendon stretches into your routine to maintain flexibility.
- Strengthen Supporting Muscles: Strength training for the calf and lower leg muscles helps to support the Achilles tendon.
- Gradual Activity Progression: Increase the intensity and duration of physical activities slowly to avoid overloading the tendon.
- Wear Appropriate Footwear: To reduce stress on the heel and tendon, wear shoes with proper arch support and cushioning.
- Manage Body Weight: Maintaining a healthy weight reduces the load on the tendon.
- Cross-Train: Include low-impact activities like swimming or cycling to balance tendon use and allow recovery.
- Listen to Your Body: Avoid pushing through pain during exercise, and rest adequately after intense activities.
Types of Insertional Achilles Tendinopathy
Insertional Achilles tendinopathy can be categorised into the following types based on the nature and progression of the condition:
- Acute Insertional Achilles Tendinopathy: This type develops suddenly and is often triggered by an abrupt increase in activity or trauma.
- Symptoms include localised pain, swelling, and tenderness at the insertion site.
- Chronic Insertional Achilles Tendinopathy: A more gradual onset, often due to repetitive stress or degeneration over time. It may involve structural changes, such as thickening of the tendon and calcification and bone spur formation.
Stages of Insertional Achilles Tendinopathy
Insertional Achilles tendinopathy progresses through the following stages:
- Reactive Tendinopathy: The early phase is characterised by tendon inflammation and pain. The tendon attempts to adapt to increased load but remains structurally intact.
- Tendon Disrepair: If the load persists, the tendon fibres begin to degenerate.
- Degenerative Tendinopathy: Advanced stage with significant structural damage, including partial tears and calcification.
Diagnosis of Insertional Achilles Tendinopathy
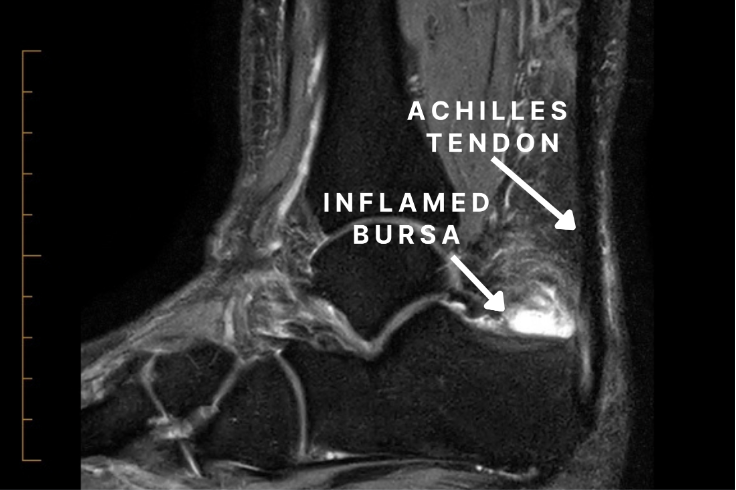
Diagnosis typically involves reviewing the patient’s history and clinical ankle examination. Imaging is required, such as:
- X-rays: To evaluate the bone structure and determine the severity.
- Ultrasound scans: Can evaluate the extent and location of disease
- MRI: Is the gold standard
Management and Treatment of Insertional Achilles Tendinopathy
Most patients will improve with non-operative management.
Options include:
- Anti-inflammatory medication: Ibuprofen should be taken in short courses and with meals, as it can irritate the belly
- Modified Footwear: Choosing shoes that do not put pressure on the spur and tendon insertion
- Podiatry and/or physiotherapy: Heel cord stretching and eccentric training, as well as modalities such as shock wave, laser or ultrasound therapy
- Surgery: For severe cases not responding to non-operative management, surgical intervention may be necessary to debride the tendon, bursa, and bone spur and repair the Achilles tendon to a healthy tendon and bone. This can include a tendon transfer to improve vascularity and push off strength in the long term (see Surgery Information: Insertional Achilles Tendinopathy)
What if Insertional Achilles Tendinopathy is Untreated?
If left untreated, insertional Achilles tendinopathy can lead to:
- Chronic Pain
- Decreased Mobility
- Tendon Rupture
- Bone Spur Formation
- Reduced Physical Activity
Early diagnosis and treatment are crucial to prevent these complications and ensure a better recovery.
